Naltrexone (Monograph)
Brand names: ReVia, Vivitrol
Drug class: Opiate Antagonists
- Alcohol Deterrents
- Deterrents, Alcohol
VA class: CN102
Chemical name: 17-(Cyclopropylmethyl)-4,5α-epoxy-3,14-dihydroxymorphinan-6-one
Molecular formula: C20H23NO4C20H23NO4•HCl
CAS number: 16590-41-3
Warning
- Hepatic Effects
-
Possible dose-related hepatotoxicity. Margin between therapeutic and hepatotoxic dosages may be less than fivefold; hepatotoxicity not apparent at usual dosages. (See Hepatic Effects under Cautions.)
-
Contraindicated in patients with acute hepatitis or liver failure; carefully weigh potential benefits against possible hepatotoxic risks in patients with active liver disease.
-
Instruct patients to discontinue naltrexone and contact a clinician if manifestations of acute hepatitis occur. (See Advice to Patients.)
Introduction
Essentially a pure opiate antagonist.
Uses for Naltrexone
Opiate Dependence
Used as an adjunct to a medically supervised behavior modification program in the maintenance of opiate cessation (opiate-free state) in individuals who were formerly physically dependent on opiates and who have successfully undergone detoxification (designated an orphan drug by FDA for this use).
Behavior modification is an integral component in maintaining opiate cessation; behavior modification programs involve supervised programs of counseling, psychologic support and therapy, education, and changes in life-style (social rehabilitation).
May diminish or eliminate opiate-seeking behavior by blocking opiate euphoria and by preventing the conditioned abstinence syndrome (i.e., heightened sensitivity to stimuli, abnormal autonomic responses, dysphoria, intense opiate craving) that occurs following opiate withdrawal.
Efficacy in maintaining long-term cessation appears to be low; poor compliance appears to be the major limiting factor. Because noncompliance with naltrexone is not associated with unpleasant symptoms of withdrawal, compliance depends more on voluntary efforts; successful cessation may be more likely in highly motivated individuals.
Because of potential for relapse to opiate use and subsequent opiate overdosage, routinely discuss availability of the opiate antagonist naloxone with all patients receiving new or reauthorized prescriptions for medications for treatment of opiate use disorder (OUD); strongly consider prescribing naloxone for use in the event of an overdose in all such patients.
Has been used for rapid or ultrarapid detoxification in the management of opiate withdrawal† [off-label] in opiate-dependent individuals, both in inpatient and outpatient settings.
Rapid opiate detoxification involves the administration of opiate antagonists (e.g., naltrexone and/or naloxone) to shorten the time period of detoxification.
Ultrarapid detoxification is similar but involves the administration of opiate antagonists while the patient is sedated or under general anesthesia. Consider the risk of adverse respiratory and cardiovascular effects associated with this procedure, as well as the costs of general anesthesia and hospitalization.
Alcohol Dependence
Management of alcohol dependence in conjunction with a behavior modification program involving supervised programs of counseling, psychologic support and therapy, and education and changes in life-style (social rehabilitation).
Used IM in individuals who are able to abstain from alcohol in an outpatient setting and are abstinent when treatment is initiated.
Behavior modification is an integral component in maintaining alcohol cessation; naltrexone has not been shown to provide any therapeutic benefit except as part of an appropriate plan of addiction management.
When used in conjunction with behavior modification, naltrexone reportedly decreases alcohol craving, reduces alcohol consumption, decreases the number of drinking days, maintains abstinence from alcohol ingestion, and prevents, decreases, or ameliorates the severity of relapse.
Naltrexone is not uniformly effective; the expected effect is a modest improvement in the outcome of conventional therapy.
Naltrexone Dosage and Administration
General
REMS for Parenteral Naltrexone
-
FDA required and approved a Risk Evaluation and Mitigation Strategy (REMS) for parenteral naltrexone.
The REMS requires that a medication guide be given to the patient each time parenteral naltrexone is dispensed; the goal is to inform patients about serious risks associated with parenteral naltrexone. (See Advice to Patients and also see Cautions.)
Verification of Opiate Abstinence Prior to Initiation of Therapy
-
Patients who are physically dependent on opiates should complete detoxification prior to initiation of naltrexone therapy.
-
Manufacturers recommend that at least 7–10 days elapse between discontinuance of opiates and initiation of naltrexone therapy because of the risk of precipitating opiate withdrawal (see Accidental Precipitation of Withdrawal under Cautions.) This waiting period may vary depending on the dose and duration of action of the opiate; allow at least 7 days in patients using relatively short-acting opiates (e.g., heroin, hydromorphone, meperidine, morphine) and at least 10–14 days in those using longer-acting opiates (e.g., methadone).
-
Some clinicians have cautiously precipitated withdrawal using repeated naloxone injections and then rapidly initiated naltrexone therapy with incremental doses of the drug; this procedure can reduce the transition period from opiate dependence to naltrexone maintenance and generally is well accepted by patients.
-
In addition to patient verification of abstinence from opiates, perform urinalysis after the minimum 7- to 10-day waiting period, but prior to administration of naltrexone, to confirm the absence of opiates. If it is uncertain whether the patient is opiate free, perform a naloxone challenge test prior to administering naltrexone.
Naloxone Challenge Test
-
Perform test prior to induction of naltrexone therapy in patients formerly physically dependent on opiates who have completed detoxification and in those suspected of having been dependent on opiates.
-
Test should not be performed in patients who are exhibiting signs and/or symptoms of opiate withdrawal, those whose urine shows evidence of opiates, or those in whom there is a high degree of suspicion that opiates are still being used, since naloxone may precipitate potentially severe opiate withdrawal.
-
Do not attempt naltrexone therapy if signs and/or symptoms of opiate withdrawal (e.g., nasal stuffiness, rhinorrhea, lacrimation, yawning, sweating, tremor, abdominal cramps, vomiting, piloerection, myalgia, skin crawling) are evident following administration of the naloxone challenge test; instead, repeat the naloxone challenge test in 24 hours.
-
Naloxone may be administered IV or sub-Q in the challenge test.
-
IV challenge test: Draw 0.8 mg of naloxone hydrochloride into a syringe. Administer 0.2 mg initially; while the needle remains in the vein observe the patient for 30 seconds for evidence of opiate withdrawal. Alternatively, some clinicians recommend 15 minutes for the period of observation. If no evidence of withdrawal is observed, inject the remaining 0.6-mg dose and observe the patient for an additional 20 minutes for evidence of withdrawal.
-
Sub-Q challenge test: Draw 0.8 mg of naloxone hydrochloride into a syringe. Inject the entire 0.8-mg dose and observe the patient for 20 minutes for evidence of opiate withdrawal.
-
If evidence of opiate withdrawal is present, delay naltrexone therapy and repeat the naloxone challenge test in 24 hours with the 0.8-mg dose; repeat the test every 24 hours until results are negative.
-
If it is uncertain whether the patient is opiate free or is undergoing opiate withdrawal following an initial test, repeat the naloxone challenge test with a 1.6-mg IV dose.
Administration
Administer orally or by IM injection.
Do not administer parenteral preparation by IV or sub-Q injection; do not administer into fatty tissue.
Oral Administration
Administer orally; minimize adverse GI effects by taking with food or antacids or after meals.
Patients should take naltrexone as directed and not attempt self-administration of opiates during therapy with the drug. (See Risks Associated with Self-administration of Opiates During Naltrexone Therapy under Cautions.)
IM Administration
IM preparation may be used in individuals who are able to abstain from alcohol in an outpatient setting and are abstinent when treatment is initiated.
Administer by deep IM injection into the upper outer quadrant of the gluteal muscle every 4 weeks (or once a month); alternate buttocks for subsequent injections.
Administer only with needle and other components of dose pack supplied by manufacturer.
Use aspiration to avoid inadvertent injection into a blood vessel.
Do not administer by IV or sub-Q injection; do not inadvertently administer into fatty tissue. Inadvertent sub-Q injection may increase likelihood of severe injection site reactions. (See Local Reactions under Cautions.)
Evaluate the patient's body habitus prior to each injection to ensure that the 1.5-inch needle supplied by the manufacturer is adequate for gluteal IM injection in that patient. Consider alternative treatment for any patient whose body habitus (i.e., gluteal fat thickness) precludes IM injection with the provided needle.
Reconstitution
Consult manufacturer’s labeling for instructions for using components of dose pack for reconstitution.
Allow dose pack to reach room temperature before reconstituting.
Reconstitute vial labeled as containing 380 mg of naltrexone extended-release microspheres with 3.4 mL of diluent; shake vigorously for 1 minute. Use only the diluent supplied by the manufacturer. Administer immediately.
Dosage
Available for oral administration as naltrexone hydrochloride; dosage expressed in terms of the salt.
Available for IM administration as naltrexone.
Adults
Opiate Dependence
Induction of Therapy for Opiate Cessation
OralInitiate induction regimen following completion of opiate detoxification and verification that the patient is free of opiates. (See General under Dosage and Administration.)
Initially, 25 mg; if no evidence of withdrawal is present, begin 50 mg daily.
Alternatively, some clinicians have administered 12.5 mg initially, followed by incremental increases of 12.5 mg daily until the usual dosage of 50 mg daily has been achieved.
Maintenance Therapy for Opiate Cessation
Oral50 mg daily following induction of therapy.
Alternatively, flexible dosing schedules have been suggested in an attempt to improve compliance. Administration of larger doses at longer intervals (e.g., 48–72 hours) may reduce opiate antagonist activity somewhat, but may improve compliance. Single doses >50 mg may increase risk of hepatic injury; weigh possible risks against probable benefits of flexible dosing.
- Flexible Naltrexone Hydrochloride Dosing Schedules for Maintenance Therapy for Opiate Cessation
-
50 mg daily Monday through Friday and 100 mg on Saturday
-
100 mg every other day
-
150 mg every third day
-
100 mg on Monday and Wednesday and 150 mg on Friday
-
150 mg on Monday and 200 mg on Thursday
Ingestion of the naltrexone dose generally should be observed in a clinic setting or by a responsible family member to ensure compliance, in which case, regimens requiring less frequent visits may be more acceptable to the patient.
Monitor patient compliance by random testing of urine for naltrexone and 6-β-naltrexol or for the presence of opiates.
Optimum duration of maintenance therapy not established; base on individual requirements and response.
In patients who discontinue naltrexone prematurely and then desire to resume therapy following a relapse to opiate abuse, perform urinalysis for the presence of opiates and, if necessary, a naloxone challenge test prior to resuming therapy. If there is evidence of opiate dependence, conduct detoxification prior to reinitiation of naltrexone therapy.
Opiate Detoxification† [off-label]
OralVarious dosage regimens have been used for rapid or ultrarapid detoxification† [off-label] of opiate dependence.
The following regimen of naltrexone, given in conjunction with clonidine to attenuate withdrawal manifestations, has been studied.
|
Day of Detoxification Therapy |
Clonidine Hydrochloride |
Naltrexone Hydrochloride |
|---|---|---|
|
Day 1 |
0.005 mg/kg initially; then titrated according to the severity of withdrawal and the adverse effects induced by clonidine |
|
|
Day 2 |
Administered every 4 hours to attenuate the withdrawal induced by naltrexone |
Administered every 4 hours; 1 mg initially; then increased in 1-mg increments during the daytime on day 2 |
|
Day 3 |
Administered every 4 hours to attenuate the withdrawal induced by naltrexone; highest mean dosage was 2.3 mg daily on day 3 |
Administered every 4 hours; dosage increased in 2-mg increments during the daytime on day 3 |
|
Day 4 |
Administered only as needed to reduce signs and symptoms of withdrawal |
10 mg 3 times daily |
|
Day 5 |
Administered only as needed to reduce signs and symptoms of withdrawal |
50 mg once daily |
Alcohol Dependence
Oral
50 mg once daily, following verification that the patient is free of opiates. (See General under Dosage and Administration.)
Optimum duration of therapy not established; safety and efficacy established only in short-term (up to 12 weeks) studies.
IM
380 mg every 4 weeks or once a month following verification that the patient is free of opiates. (See General under Dosage and Administration.)
If a dose is missed, reschedule administration with a health-care professional as soon as possible.
Therapy may be initiated with parenteral preparation; not necessary to initiate therapy with oral naltrexone and then switch to parenteral preparation.
Special Populations
Hepatic Impairment
Alcohol Dependence
IM
Dosage adjustment not needed in patients with mild to moderate (Child-Pugh class A or B) hepatic impairment.
Renal Impairment
Alcohol Dependence
IM
Dosage adjustment not needed in patients with mild renal impairment (Clcr of 50–80 mL/minute).
Cautions for Naltrexone
Contraindications
-
Patients receiving opiate agonists (except for emergency situations).
-
Nondetoxified patients physically dependent on opiates, including those receiving maintenance treatment with opiates (e.g., methadone).
-
Patients experiencing acute opiate withdrawal.
-
Patients who experience opiate withdrawal following administration of the naloxone challenge test or in patients in whom urinalysis for the presence of opiates is positive.
-
Patients with acute hepatitis or hepatic failure.
-
Patients with known hypersensitivity to the drug or any ingredient in the formulation. Not known whether cross-sensitivity exists between naltrexone and naloxone or phenanthrene-derivative opiate agonists (e.g., codeine, morphine, oxymorphone).
Warnings/Precautions
Warnings
Hepatic Effects
Possible dose-related hepatocellular injury, manifested as increases in serum hepatic enzyme concentrations. (See Boxed Warning.)
Manufacturers state that naltrexone-induced hepatocellular injury appears to be a direct toxic rather than an idiosyncratic effect. Some clinicians suggest that liver function abnormalities may be caused by noroxymorphone, a minor metabolite of naltrexone that has opiate agonist activity.
Manufacturer of oral naltrexone recommends monitoring liver function at intervals deemed appropriate for the naltrexone dosage employed and the clinical status of the patient.
Local Reactions
IM injection associated with injection site reactions (e.g., tenderness, induration, pain, pruritus, ecchymosis, nodules, swelling) in most patients. Cellulitis, hematoma, abscess, sterile abscess, and necrosis also reported. Injection site reactions occur predominantly in females.
Some reactions may be very severe, result in substantial scarring, or require surgery, including debridement of necrotic tissue. Inadvertent sub-Q injection may increase likelihood of a severe injection reaction.
Patients should monitor the injection site and contact clinician if injection site reactions worsen or persist. (See Advice to Patients.) Promptly evaluate patients with signs of abscess, cellulitis, necrosis, or extensive swelling to determine if referral to a surgeon is warranted.
Verification of Opiate Abstinence Prior to Initiation of Therapy
Naltrexone may precipitate mild to severe withdrawal in patients physically dependent on opiates.
To minimize the risk of precipitating signs and symptoms of withdrawal, instruct opiate-dependent individuals who are candidates for naltrexone therapy to remain free of opiates for a minimum of 7–10 days prior to initiating therapy with the drug.
Absence of opiates in urine is frequently insufficient evidence that a patient is free of opiates. If it is uncertain whether the patient is opiate free, perform a naloxone challenge test prior to administering naltrexone. (See Naloxone Challenge Test under Dosage and Administration.)
Risks Associated with Self-administration of Opiates During Naltrexone Therapy
Self-administration of large doses of opiates in an attempt to overcome the antagonist activity of naltrexone may produce signs and symptoms of acute opiate overdosage (e.g., respiratory arrest, circulatory collapse, death).
Signs and symptoms of opiate overdosage also may occur following administration of smaller doses of opiate agonists relatively long after the last naltrexone dose or in an amount that results in a longer duration of agonist activity than the antagonist activity of naltrexone and its metabolites.
Advise patients of the serious consequences of self-administration of opiates during naltrexone therapy. (See Advice to Patients.)
Eosinophilic Pneumonia
Eosinophilic pneumonia reported rarely in patients receiving parenteral naltrexone. Consider eosinophilic pneumonia in patients with pneumonia who have not responded to anti-infective therapy.
General Precautions
Therapeutic Use of Opiates in Naltrexone-treated Patients
In an emergency situation when adequate analgesia can be achieved only by administration of an opiate agonist in naltrexone-treated patients, cautious administration of an opiate may afford adequate analgesia, but higher than usual dosages may be required. Whenever possible, use nonopiate analgesics, regional analgesia, conscious sedation with a benzodiazepine, or general anesthesia.
If an opiate is required as a component of anesthesia or analgesia, the patient should be continuously monitored in an anesthesia care setting by individuals who are trained in the use of anesthetic agents and in the management of respiratory depressant effects of potent opiates and who are not involved in the conduct of the surgical or diagnostic procedure.
Respiratory depression produced by the opiate may be deeper and more prolonged. Patients may experience apparent nonopiate receptor-induced effects such as facial swelling, pruritus, generalized erythema, or bronchoconstriction that are probably caused by opiate-induced histamine release and/or other mechanisms.
Use of a short-acting opiate with minimal respiratory depression is preferable; adjust dosage of the opiate agonist carefully according to individual requirements and response. Closely monitor the patient in a setting equipped and staffed by health-care personnel appropriately trained in CPR.
Discontinue oral naltrexone ≥48 hours prior to elective surgical procedures requiring opiate analgesia.
Avoid use of other opiate-agonist-containing preparations (e.g., those used for the management of cough or diarrhea) when alternative nonopiate therapy is available, since adequate therapeutic benefit may be difficult to achieve with an opiate.
Accidental Precipitation of Withdrawal
Accidental ingestion of naltrexone has precipitated severe withdrawal in some patients physically dependent on opiates; signs and symptoms of withdrawal usually appeared within 5 minutes of naltrexone ingestion and continued for up to 48 hours.
Suicide
Increased risk of suicide in substance abusers with or without depression; risk is not abated by naltrexone therapy.
Individuals with Bleeding Disorders
Use IM preparation with caution in individuals with thrombocytopenia or a coagulation disorder (e.g., hemophilia).
Specific Populations
Pregnancy
Category C.
Not known whether naltrexone affects the duration of labor and delivery.
Lactation
Naltrexone and the active metabolite (6-β-naltrexol) are distributed into human milk. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy not established in children <18 years of age.
Hepatic Impairment
Contraindicated in patients with acute hepatitis or hepatic failure. (See Boxed Warning and see Hepatic Effects under Cautions.)
Use with caution in patients with hepatic impairment. When administered orally, possible increased systemic exposure to the drug.
Renal Impairment
Use with caution in patients with moderate to severe renal impairment.
Common Adverse Effects
Treatment of opiate dependence: insomnia, anxiety, nervousness, abdominal pain and cramps, nausea, vomiting, fatigue, joint and muscle pain, headache.
Treatment of alcohol dependence: nausea, headache, dizziness, nervousness, fatigue, insomnia, vomiting, anxiety, somnolence, injection site reaction.
Drug Interactions
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Clonidine |
Concomitant administration may reduce the duration of opiate withdrawal by decreasing opiate-induced postsynaptic supersensitivity |
|
|
Disulfiram |
Both drugs are potentially hepatotoxic |
Manufacturers recommend concomitant use only if the potential benefits justify the possible risks |
|
Opiate agonists |
Patients receiving naltrexone may not benefit therapeutically from opiate-containing preparations, including those used for the management of cough and cold, diarrhea, and pain Naltrexone can precipitate potentially severe opiate withdrawal |
Avoid use of opiate-containing preparations during naltrexone therapy when alternative nonopiate therapy is available Avoid use of naltrexone in patients receiving opiates or in nondetoxified patients physically dependent on opiates |
|
Phenothiazines (thioridazine) |
Possible increased lethargy and somnolence |
|
|
Tests, urinary opiates |
Possible interference with some enzymatic assays for opiates No interference reported with thin-layer (TLC), gas-liquid (GLC), or high-performance liquid (HPLC) chromatography assays for methadone or morphine |
|
|
Tests, urinary quinine |
No interference reported with TLC, GLC, or HPLC methods |
Naltrexone Pharmacokinetics
Absorption
Bioavailability
Rapidly and almost completely (about 96%) absorbed following oral administration, but undergoes extensive first-pass metabolism in the liver; only 5–40% reaches systemic circulation unchanged.
Peak plasma concentrations of naltrexone and the active metabolite (6-β-naltrexol) usually occur within 1 hour following oral administration.
Following IM administration of the extended-release injection, naltrexone is released slowly and gradually from the microspheres by diffusion and erosion as the polylactide co-glycolide polymer degrades. Peak plasma concentrations of naltrexone and the active metabolite (6-β-naltrexol) occur in about 2–3 days; steady-state plasma concentrations of naltrexone and 6-β-naltrexol are attained by the end of the dosing interval after the first injection.
Following administration of a single IM dose of naltrexone 380 mg, total naltrexone exposure is three- to fourfold higher and 6-β-naltrexol exposure is 3.4-fold lower than exposure following oral administration of naltrexone 50 mg daily for 28 days.
Onset
Onset of opiate antagonism occurred 15–30 minutes following oral administration in a limited number of patients who had been receiving morphine chronically.
Decreases opiate craving within 3–5 weeks after start of oral naltrexone in individuals formerly dependent on opiates; reduction in opiate craving has occurred during the first week of therapy in some individuals, with further decreases occurring in subsequent weeks.
Duration
Duration of opiate antagonist activity appears to be dose dependent and is longer than that of equipotent doses of naloxone.
Special Populations
Changes in oral bioavailability appear to be related to severity of liver disease. AUC increased 5- or 10-fold in patients with compensated or decompensated cirrhosis, respectively.
Following IM administration, plasma concentrations of naltrexone and 6-β-naltrexol in individuals with mild to moderate hepatic impairment (Child-Pugh class A and B) are similar to those in healthy individuals with normal hepatic function.
Distribution
Extent
Widely distributed throughout the body; considerable interindividual variation in distribution parameters during the first 24 hours following a single oral dose.
Not known whether naltrexone and/or its metabolites cross the placenta. Naltrexone and 6-β-naltrexol are distributed into human milk.
Plasma Protein Binding
Approximately 21–28%.
Elimination
Metabolism
Metabolized in the liver principally by reduction of the 6-keto group of naltrexone to an active metabolite, 6-β-naltrexol (6-β-hydroxynaltrexone); other minor metabolites are formed.
Because oral but not IM administration of naltrexone results in substantial first-pass hepatic metabolism, 6-β-naltrexol concentrations following IM administration are substantially lower than concentrations achieved following oral administration.
Naltrexone and its metabolites may undergo enterohepatic circulation.
Elimination Route
Excreted principally in urine via glomerular filtration, mainly as metabolites (unconjugated and conjugated).
Half-life
Following oral administration, biphasic.
Initial phase, oral administration: 1.1–3.9 hours for naltrexone; 2.3–3.1 hours for 6-β-naltrexol.
Terminal phase, oral administration: 9.7–10.3 hours for naltrexone; 11.4–16.8 hours for 6-β-naltrexol.
Following IM administration, half-life of naltrexone and 6-β-naltrexol is 5–10 days.
Special Populations
Following IM administration, pharmacokinetics not altered in patients with mild renal impairment (Clcr of 50–80 mL/minute).
Stability
Storage
Oral
Tablets
20–25°C.
Parenteral
Extended-release Injection
Store entire dose pack at 2–8°C. May be stored at temperatures not >25°C for ≤7 days prior to administration. Do not freeze.
After mixing with diluent, use immediately.
Actions
-
Essentially a pure opiate antagonist.
-
Opiate antagonist activity on a weight basis is reportedly 2–9 times that of naloxone.
-
In usual doses in patients who have not recently received opiates, naloxone exerts little or no pharmacologic effect.
-
In patients who have received single or repeated large doses of opiate agonists, naltrexone attenuates or produces a complete but reversible block of the pharmacologic effects (e.g., physical dependence, analgesia, euphoria, tolerance) of the opiate.
-
Antagonizes most of the subjective and objective effects of opiates, including respiratory depression, miosis, euphoria, and drug craving.
-
Because the duration of action of naltrexone may be shorter than that of the opiate, the effects of the opiate may return as the effects of naltrexone dissipate. Degree of opiate antagonism produced by naltrexone depends on the dose and the time elapsed since the last dose of naltrexone and the dose of the opiate.
-
Does not produce physical or psychologic dependence, and tolerance to the drug’s opiate antagonist activity reportedly does not develop. May precipitate mild to potentially severe withdrawal in individuals physically dependent on opiates or pentazocine.
-
Is thought to act as a competitive antagonist at µ, κ, and δ receptors in the CNS; appears to have the highest affinity for the μ receptor.
-
Alcohol ingestion stimulates release of endogenous opiate agonists, which may increase some of the rewarding effects associated with alcohol ingestion through agonist activity at opiate (e.g., μ) receptors. By competitively binding to opiate receptors, naltrexone may reduce alcohol consumption by blocking the effects of endogenous opiates and thus making alcohol ingestion less pleasurable.
-
Does not cause disulfiram-like reactions following ingestion of alcohol.
Advice to Patients
-
Importance of patient reading the medication guide prior to initiating parenteral naltrexone therapy and before each injection of the drug. Importance of ensuring that patient understands risks.
-
Importance of patients informing clinicians that they are taking naltrexone. Advise patients to carry a medical identification card that can alert clinicians to this fact in an emergency situation.
-
Importance of contacting a clinician if manifestations of acute hepatitis (e.g., abdominal pain lasting more than a few days, light-colored [e.g., white] stools, dark urine, yellowing of the eyes) occur. Discontinue oral naltrexone.
-
Importance of not self-administering opiates (e.g., heroin) during naltrexone therapy, since self-administration of small doses of opiates in an attempt to overcome the antagonist activity of naltrexone will not result in any pharmacologic effect and large doses may result in serious consequences (e.g., coma, death).
-
Advise patients that they may be more sensitive to lower doses of opiate agonists following discontinuance of naltrexone therapy.
-
Because of potential for relapse to opiate use and subsequent opiate overdosage, advise patients of the benefits of naloxone following opiate overdose and of their options for obtaining the drug.
-
Advise patients receiving parenteral naltrexone to contact clinician if manifestations of pneumonia (shortness of breath, cough, wheezing) occur.
-
Advise patients receiving parenteral naltrexone to monitor the injection site and to contact clinician if injection site reactions (i.e., pain, swelling, tenderness, induration, bruising, pruritus, redness) worsen or if they do not improve within 2 weeks following injection. Advise patients to notify clinician promptly if intense or prolonged pain, swelling, skin color changes, or signs of necrosis (e.g., hard nodule, blistering, open wound, dark scab) are present at the injection site.
-
Advise patients that they may need to be referred to a surgeon for worsening injection site reactions.
-
Risk of dizziness; avoid driving or operating heavy machinery until effects on the individual are known.
-
Potential for depression and suicidality to occur; importance of contacting clinician immediately if new or worsening symptoms of depression or suicidal thoughts occur.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses (e.g. liver disease).
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
For injectable suspension, extended-release, for IM use |
380 mg |
Vivitrol (available as a dose pack containing naltrexone microspheres, diluent, needles) |
Alkermes |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
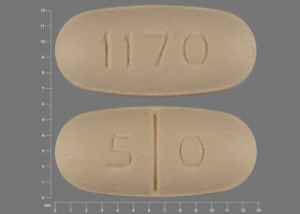
Oral |
Tablets |
50 mg* |
Naltrexone Hydrochloride |
|
|
Tablets, film-coated |
50 mg* |
Naltrexone Hydrochloride |
||
|
ReVia (scored) |
Duramed |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions July 19, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Frequently asked questions
- What is low dose naltrexone (LDN)?
- What happens if you drink alcohol while taking naltrexone?
- What to avoid when taking naltrexone?
- Should I take naltrexone in the morning or at night?
- Does naltrexone cause weight gain?
- Acamprosate vs naltrexone: How do they compare?
- How does naltrexone make you feel?
- How long does naltrexone take to work?
- What is the mechanism of action for naltrexone?
More about naltrexone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (591)
- Drug images
- Latest FDA alerts (1)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: antidotes
- Breastfeeding